|
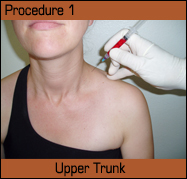
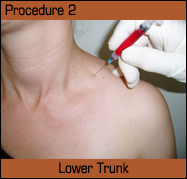
Lecture at WUSM WASHINGTON UNIVERSITY SCHOOL OF MEDICINE When symptoms in neurogenic thoracic-outlet syndrome (NTOS) become refractory to the usual pharmaceuticals, appropriate physical therapy, or surgical interventions, we now have two neuroprotective agents, widely used in other disorders, that can improve symptoms in these difficult to treat patients. The first of these is heparin, working through mechanisms that are novel in the context of chronic pain, but intensively investigated and effectively applied in treating other disorders. My interest in heparin is the result of ongoing work trying to understand some of the basic mechanisms operant in chronic pain. Some time ago I began working with a vascular surgeon at UCSF to better understand NTOS, a disorder with very interesting, but complex, and, at times, seemingly contradictory presentations. My curiosity had been piqued by the often dramatic postoperative improvement of not only arm pain, but also frequently jaw, ear, head, and low back pains, not to speak of paresthesias. Additionally, CRPS-like hyperesthesias, cold sensitivity, as well as suboccipital radiating migrainoid headaches disappeared or were much improved. The same was true for the frequent gastrointestinal disorders that seem to accompany this syndrome. Such diversity was intriguing on its own and prompted a search for commonality. Given the often diffuse seeming symptomatology with its wide range of affected nerves and nerve fields, we thought that using intraoperative thermography during thoracic outlet decompressions might provide more information about the specific irritants that were causing such painful and widespread neural dysfunction.. Intraoperative thermography monitored the decompression by imaging the exposed dorsum of the affected hand using on-line infra-red video cameras, exhibiting a clear-cut dermatomal distribution. The affected hands were 2-5 What we found was that the usual suspects (scalenes, fibrous interdigitations, enlarged lateral processes) certainly played a consistent and significant role, but that the bulk of the thermal normalization occurred following resection of small, adherent, fibrotic matrices, usually done as part of the neurolysis. Fibrotic tissue is usually thought of as pharmacologically inert, causing problems of constriction and pain directly by mechanical strangulation of the affected nerves. The epi- or perineural fibrotic scar that the vascular surgeon was removing, however, turned out to be pharmacologically very active with multiple pro-inflammatory neuropeptides secreted by a rich matrix of largely immature neurites traversing the fibrosis. This was determined by immunoassay at UCSF and histology at UCLA. Most of the time there was little evidence of a direct mechanical effect. The closest analogous description that I could find in the literature was that of painful hypertrophic scarring, which showed a similar inflammatory neuropeptide distribution and an abundance of growth factors that were also pro-inflammatory (NGF, FGF…), at least in part. In fact, this comparison to hypertrophic scarring did not seem far fetched when observing the extensive fibrosis often present in surgical re-dos. This again emphasized the importance of neuronal secretions and elaborations of inflammatory substances and growth factors. Our observations, both clinically and histologically, led to our considering NTOS as a disorder of neurogenic inflammation. The driving force behind the disease becomes the recurrent progressive and atypical inflammation with its attendant proliferation. This inflammation is atypical because the cardinal signs (calor, rubor, tumor, dolor, and functio laesa) are not always manifest nor does it respond to the usual anti-inflammatories. One only needs to see the edematous and inflamed state of the operated on nerve trunks to be convinced of the significance of inflammation in this disorder. The geometric development of this neurogenic inflammation accounts for the non-linear (more or less sudden) increase and/or spread of symptoms that occurs so typically once the symptoms become entrenched. The consequent cytokine elaboration sensitizes not only the local trunks, but also those near enough to be involved deleteriously by diffusion. These include the recurrent laryngeal, vagus, autonomic ganglia and, over time, more distant spread to involve adjacent trunks. Subsequent distal sensitization by neurally activated cytokines predisposes to the frequent occurrence of double and triple crush injuries, and eventually can affect the spinal cord as is suggested by the appearance of mirror symptoms and subsequent soft neurological findings of intermittent motor dysfunction, as well as evolving distant pain and paresthesias. Extensive work has underscored the importance of cytokine driven inflammatory processes that are Cox 1 and 2 independent as being responsible for sensitizing nerves, initiating and perpetuating much of neuropathic pain. It is these cytokines, of which TNF alpha is probably the most notorious, that sensitize the tissues adjacent to the small initial lesions, subsequently spreading through a variety of mechanisms perpetuated by recurrent injury and inflammation. This neural sensitization also explains the generally absent “objective” indicators when using electrodiagnostics or conventional imaging. Given the lack of obvious neuronal cell death (as evidenced by these frequent negative findings), in many, if not most, cases apoptosis seems not to be a major issue in NTOS. Neural dysfunction, however, is. I thought that anything that could improve the neurogenically induced fibrosis, inflammation and local vasospasm would be of help clinically. As a result, I turned to heparin with its recognized effects of decreasing collagen cross linking and of stabilizing the vascular system. I started with 1,000 units, injected perineurally about the relevant brachial plexus trunks. Quite surprisingly, this dramatically reduced painful symptomatology and I eventually performed a controlled clinical study in which thirty subjects with entrapments participated. Injections of perineural unfractionated heparin resulted in an over 40% reduction in pain within 36 hr. This turned out to be cumulative and the completion of a series of six weekly injections gave an average of over 80% pain relief. This result is tempered by the observation that the patients continued to be vulnerable to easy re-injury, but did experience significant pain amelioration. Heparin is truly pleiotropic, affecting not only coagulation at multiple points, but also controlling mast cells, monocytes, the complement cascade, smooth muscle proliferation, NO production, and is considered generally cytoprotective. For its affects on neuropathic pain in NTOS, we need to look more specifically at its anti-inflammatory activity, which has been found useful in asthma, adult respiratory distress syndrome, ulcerative colitis, rheumatoid arthritis, myocardial infarction, severe burns, and radiation-induced neuropathy. The proposed mechanisms for this are quite complex and involve intraneural/resident mast cells, monocytes, fibroblasts, followed by modulation of the panoply of inflammatory cells and factors impacting once the local endothelium is breached. Interestingly, the significant delay following Heparin injection before symptoms improve, which is usually 24-36 hr., suggests that the anti-inflammatory activity and resultant pain reduction are a function of heparin working largely as a transcription factor in inducing the production of new controlling elements. Heparin has been documented as modulating NF-kB. The procedure itself is very straight forward. I expand 1 ml of 5,000 units of heparin per ml with a further ml of B12 and one of 1% Lidocaine to a final 3 ml contained in a 3 ml, 25-gauge, 1 ½” syringe. The consequent bolus injected is a little bit over 800 units per ½ ml, which is the standard amount that I use. One penetrates the skin at roughly a 30
These injections have proven to be very safe, straight forward, and effective. The critical task for optimal relief is the anatomically appropriate placement of the heparin bolus to where it is, in fact, needed. This is of critical importance. The importance of the placement is also underscored when treating other neuropathic disorders. I have been using this methodology for well over a decade with a continued excellent response and no significant side effects. Patients do report, after the injection, a dull aching sensation at the site for the first 24 hr., followed by substantial pain relief, which can last up to six months or even longer. The majority of patients, over time, become relatively symptom free, doing well on conservative regimens and requiring further treatment only when severely flared up. There is a core group of severely afflicted patients, most of whom are failed surgical decompressions, who require treatment every two weeks or so. At this point, having achieved decent pain control, I felt that the primary problem was one of finding some way to affect these immature, innervated bits of fibrotic tissue that directly afflicted nerves neurohumorally in such an adverse fashion. This was especially evident in patients who have had just too much inflammatory damage accumulated over too many reinjuries. For example, despite anti-nociception from heparin, attempting to open a pasta sauce bottle can cause a flare-up lasting days to weeks, implying that the fundamental pathologic mechanism remains in place. What do we know about this mechanism? It must be primarily neural involving sensitized nervi-nervorum and communicating with local mast cells, monocytes, and fibroblasts to participate in the micro-inflammatory process that drives the pathology. This involves not only inflammation, but also the accompanying growth factors, which affect nerves, muscles (hence, the frequent scalene hypertrophy), existing fibrosis, as well as irritating nearby nerves, such as the vagus and, ultimately, the spinal cord (not to even mention activating the local innate immune response) to produce the insidious, cumulative, and devastating symptoms typical of NTOS. Given the immature state of these hypersensitive, sprouting nerves, the supposition that they are the result of a process of dedifferentiation becomes very attractive. We now know, with the last decade or so of work on stem cells, that dedifferentiation is possible. This allows us to consider the possibility that if it’s as sensitive as an immature nerve, looks like one, and controls similar functions, then it is one. Given the paucity of neuronal death (consistently normal findings on elecrodiagnostics), this leaves dedifferentiation as a reasonable explanation. I hypothesize that local neuronal dedifferentiation results in a mechanically and thermally hypersensitive phenotype, causing the pain and dysfunction of NTOS. As a result, I started looking for something that might induce differentiation and was safe to use clinically. What I found was erythropoietin (EPO), which, at that point, was described as very safe and a substance that was neuroprotective, as well as an inducing neural differentiation. After consultation with a number of kidney specialists (the drug is used primarily in kidney failure), and some anecdotal results, I put together a small clinical study on the effects of very low-dose and perineurally applied EPO. From previous work, we know that EPO can ameliorate neuronal injury, improve neuronal function, promote the integrity of the blood brain barrier, and induce (either directly or indirectly) multiple growth factors. It also activates Schwann cells, decreases monocyte infiltration, and modulates astrocyte activity. Possibly more significantly, it inhibits multiple kinases and nuclear factors with the subsequent induction and modulation of corresponding transcriptional factors. Function can be dramatically improved in cerebral focal ischemia, neonatal hypoxia, subarachnoid hemorrhage, and glutamate neurotoxicity. Unfortunately, this requires rather heroic doses of over 60,000 units of EPO per week. My experience with heparin led me to attempt low-dose, locally administered infiltration and, accordingly, I used 1,000 units, as described for the heparin injections, about the upper and lower trunks. These injections were repeated once per month for two subsequent months and then the patients followed for six months. I found that 54% of the patients had greater than 80% reduction in pain which remained constant throughout the follow-up period without the vulnerability to easy reinjury that was present with heparin treatment. Thus, the majority responded with improvement in neuronal irritability, analogous to terminal differentiation, and affecting genuine curative action. Unfortunately, at this point, the FDA issued a black-box warning because of results just received, indicating that EPO caused increased mortality in cancer patients and increased blood clots systemically in other study populations. In my own population, three patients did have transient blood pressure elevations with one of them high enough to be of some concern. All resolved completely without consequences, within 24 hr., and no other side effects were noted during follow-up. Indeed, 2,000 units of EPO once per month in an, otherwise, healthy population would seem to be quite minimal. However, it is not clear if EPOs side effects are dose dependent (it seems so, but there is controversy) and, if so, to what extent. Carbamylated EPO, which is non-erythropoietic, has held out the promise of clinical use for some years, but this continues to be just a promise, given that its side effects are still undetermined. At present, the risks of EPO in otherwise, normal individuals are unknown, but, given its extensive use in the endurance athletic population with no documented side-effects, further use of EPO deserves investigation given the potential tremendous benefit for its use in painful disorders. At present, I am working on more specific instructions from the manufacturer, given the fact that the FDA has no opinion on the use of low-dose erythropoietin and sticks by its indications. There is obvious and significant promise in the use of EPO or its developed congeners. I would like to leave you with three thoughts: At present, and hypothetically, the description that seems to best fit the symptom elaboration and tissue pathology of NTOS is that of neurogenically initiated and controlled micro-inflammation that self perpetuates via neurites and dedifferentiated nervi nervorum. Next, when symptoms become intransigent, small amounts of unfractionated heparin, injected perineurally, can significantly reduce them, allowing resumption of the necessary conservative approach. Lastly, that this kind of chronic debilitating pain can be dramatically affected by agents that influence overall neuronal function, differentiation/dedifferentiation as opposed to just their synaptic regimens. This includes not only EPO, but also other potential growth and/or transcription factors, the development of which would be welcomed more generally, as well.. Biblography@www.doctorellis.com
|